Quality sleep is essential for good health, but PTSD can make it difficult to achieve. Many people don’t realize there’s a strong link between PTSD and sleep apnea, a condition that can further disrupt rest. If you’re dealing with both, you’re not alone. Understanding this connection is the first step toward finding effective treatment and getting the restorative sleep you deserve.
 Sleep apnea is a sleeping problem in which you have your breath stopping and restarting a number of times at night. Obstructive sleep apnea (OSA) is the most prevalent one. It occurs, when the muscular system of the throat relaxes excessively, clogging your air-way. Central sleep apnea is another form whereby, the brain fails to relay the right signals to the muscles that coordinate breathing.
Sleep apnea is a sleeping problem in which you have your breath stopping and restarting a number of times at night. Obstructive sleep apnea (OSA) is the most prevalent one. It occurs, when the muscular system of the throat relaxes excessively, clogging your air-way. Central sleep apnea is another form whereby, the brain fails to relay the right signals to the muscles that coordinate breathing.
Post-Traumatic Stress Disorder, also known as PTSD, is the development of a condition in the mind when a person either knows someone or has experienced a traumatic event, referred to above as accident, natural calamity, warfare, or even assault. It influences the workings of the brain in terms of memories, stress, and feelings and this may lead to flashbacks, nightmares, anxiety, inability to deal with everyday living. When it is not addressed, PTSD may influence relationship, work, and the overall quality of life.
Falling asleep and sleeping are very difficult to a wide range of the PTSD sufferers. Sleep apnea is a problem part of others.
Post-traumatic stress disorder (PTSD) and sleep apnea are often found to coexist, creating a challenging cycle that affects both mental and physical health. Research suggests that the stress and hyperarousal caused by PTSD can contribute to sleep disturbances, including obstructive sleep apnea (OSA).
When you have PTSD, your body stays on high alert, even during sleep. This constant alertness can lead to shallow sleep or waking up frequently. Add sleep apnea to the mix, and the quality of sleep becomes even worse. The two conditions can feed into each other, creating a cycle of poor rest and heightened stress.
PTSD and sleep apnea both affect how your brain and nervous system work. PTSD triggers the "fight-or-flight" response, which increases your heart rate and makes your body tense. Sleep apnea interrupts breathing, which also stresses the body and mind.
Over time, your brain begins to link sleep with fear and danger. That makes falling asleep more stressful, and staying asleep even harder.
Several factors can increase the likelihood of developing both PTSD and sleep apnea:
Living with PTSD and sleep apnea can significantly disrupt daily routines and overall well-being. These conditions often interfere with work, relationships, and physical health, creating a cycle of stress and fatigue.
Lack of sleep can make PTSD symptoms worse. If you're not getting restful sleep, you may feel more anxious, irritated, or emotionally drained during the day. This can lead to more flashbacks, mood swings, and trouble focusing.
Both PTSD and sleep apnea can increase the risk of other health issues like:
One of the most common problems faced by people with sleep apnea and PTSD is extreme tiredness during the day. This makes it hard to work, study, or do everyday tasks. It can also increase the risk of accidents, especially when driving or operating machinery.
 Managing PTSD and sleep apnea often requires a combined approach that addresses both conditions simultaneously. By incorporating lifestyle changes, medical treatments, and mental health support, individuals can improve their overall well-being and quality of life.
Managing PTSD and sleep apnea often requires a combined approach that addresses both conditions simultaneously. By incorporating lifestyle changes, medical treatments, and mental health support, individuals can improve their overall well-being and quality of life.
The first step is speaking to a healthcare provider. They may recommend:
A CPAP machine is a common treatment for sleep apnea. It helps keep your airway open while you sleep by providing constant air pressure through a mask. It may feel uncomfortable at first, but many people find it improves sleep quality over time.
Psychological therapies like Cognitive Behavioral Therapy (CBT) or Exposure Therapy can help you process trauma and reduce PTSD symptoms. Over time, this may also help improve your sleep patterns.
Simple changes to your routine can make a big difference:
Improving your overall health can also help. Consider:
If your symptoms are not improving, it’s a good idea to consult a sleep specialist or mental health professional. They can help identify underlying issues and recommend appropriate solutions. In some cases, you may need a combination of treatments, such as therapy, medication, or changes to your sleep routine.
Creating a plan tailored to your lifestyle can make all the difference. Partner with your doctor to tackle sleep problems early and boost your health and quality of life..
Living with both PTSD and sleep apnea is tough, but it’s not something you have to handle alone. These conditions often go hand in hand, but with the right treatment, support, and routine, you can take back control of your sleep—and your life. Remember, better sleep starts with small steps. Take the first one today by talking to a healthcare provider who understands both mental health and sleep disorders.

Discover how hostels make budget travel affordable, social, and unforgettable.

Discover smart and easy ways to explore your dream destinations on a budget.

Explore top travel destinations blending culture, nature, and sustainability.

Balanced nutrition supports brain health and mood. Discover how diet affects emotional well-being and mental resilience.

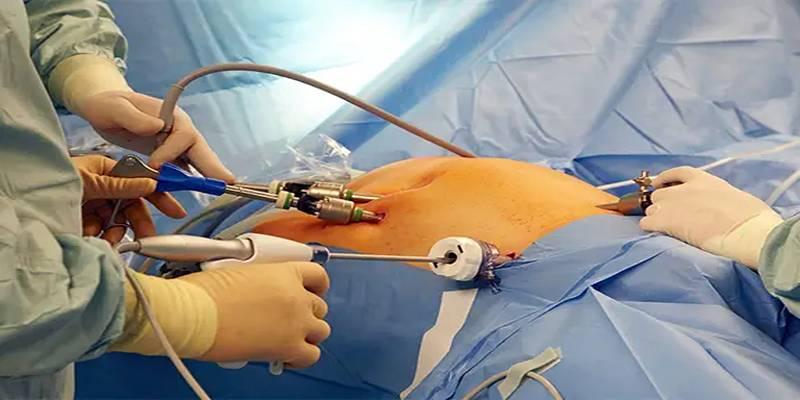
Laser eye surgery guide detailing types, risks, recovery process, candidacy factors, and costs for improved vision.

Discover 10 science-backed strategies to optimise health, enhance wellness, and maintain long-term vitality naturally.
A 40-year study reveals that weight loss surgery lowers early death risk, offering long-term health and survival benefits.

Busy parents can enjoy the holidays with quick, healthy meals that save time, reduce stress, and support family wellness.

Learn the types, causes, and treatments for headaches, and discover when it’s time to consult a healthcare professional.

Is it safe to travel to Sicily after Mount Etna’s eruption? Here’s the latest safety advice, alerts, and travel tips for visitors

Bangkok, Lima, Lyon, Wellington, Osaka, and Lucknow are the top food capitals of the world that serve you the best local flavors

Get updated travel safety tips and real-time alerts for Bali tourists following the recent volcano eruption and ash disruptions